- Over 70% of key bacteria resist standard treatments in Africa
- WHO urges urgent action to prevent global health crisis
Antibiotic resistance now affects one in five infections across Africa, surpassing the global average, where one in…
Antibiotic resistance now affects one in five infections across Africa, surpassing the global average, where one in…

RIYADH, SAUDI ARABIA, October 19, 2025 /EINPresswire.com/ — King Faisal Specialist Hospital and Research Centre (KFSHRC) has recorded exceptional kidney transplant survival rates, with one-year patient and graft survival ranging between 97…
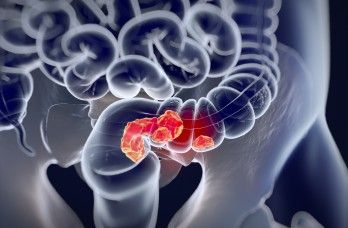
Adjuvant therapy can feasibly yield circulating tumor DNA (ctDNA) clearance in a portion of patients with colorectal cancer (CRC) and postoperative ctDNA positivity, with clearance correlating with superior disease-free survival (DFS) outcomes, according to findings from the INTERCEPT CRC study presented at the
ctDNA dynamics data after the time of surgery or ablation revealed that 69% of patients had ctDNA negativity on all tests, while 18% had positive results on all tests. Additionally, 3.1% had ctDNA clearance on at least 2 tests, 2.4% had clearance on 1 test, and 8% converted from ctDNA negativity to positivity. Furthermore, adjuvant therapy resulted in ctDNA clearance among 26% (n = 20/77) of patients with ctDNA-positive results after surgery, with 13 (17%) having clearance on at least 2 tests.
From the time of first ctDNA-positive test result in the stage I to III CRC population, DFS outcomes were significantly improved among those with clearance on at least 2 tests (P <.0001). Data revealed similarly significant outcomes among patients with stage IV disease (P <.0001).
Following adjuvant therapy, 70% of patients had ctDNA negativity on all tests, while 19% had positive results on all tests. Other data showed that 1.5% had ctDNA negativity on at least 2 tests, 1.4% had clearance on 1 test, and 9% converted from ctDNA negativity to positivity.
The study population included 403 patients who had ctDNA-positive results at any time after surgery and adjuvant treatment, with 4.2% showing at least 1 subsequent negative reading without any intervention. Furthermore, 2.1% of this population had ctDNA-negative results on at least 2 sequential tests without any intervention, and 1.7% had no recurrences at the time of follow-up. Among patients with spontaneous ctDNA clearance, the median duration of clearance was 11.2 months, and the mean tumor molecules per milliliter was 0.06 (range, 0.02-1.89).
“Adjuvant treatment can clear a quarter of the patients [who] are ctDNA positive postoperatively. Those with ctDNA clearance had superior DFS,” presenting author Emerik Osterlund, MD, PhD, a postdoctoral fellow in Gastrointestinal Medical Oncology at The University of Texas MD Anderson Cancer Center, stated in the presentation.1 “The rate and durability of [spontaneous] ctDNA clearance was very low.”
According to Osterlund, previous studies have demonstrated how ctDNA can be employed to monitor minimal residual disease, with ctDNA positivity representing a strong risk factor for disease recurrence following procedures administered with curative intent.2 However, he noted limited findings on the rates and durability of spontaneous ctDNA clearance, the process of transitioning from ctDNA positivity to negativity without any intervention. Consequently, Osterlund and colleagues aimed to evaluate the behavior and clearance of ctDNA following procedures with curative intent among patients with stage I to IV CRC.
As part of the INTERCEPT program, 1301 patients with newly diagnosed or previously treated resectable stage I to IV CRC enrolled on the study, with 53% having stage I to III disease and 47% having stage IV disease. Patients received standard-of-care therapy—surgical resection with or without neoadjuvant and adjuvant treatment—and underwent tissue collection and testing via ctDNA assays in the postoperative setting and/or following therapy. Investigators then conducted routine surveillance via imaging & labs, with ctDNA assay testing occurring approximately every 3 months at each surveillance visit.
“ctDNA clearance is useful for seeing potential benefit in novel therapeutic studies,” Osterlund concluded.1

Sucker Punch has released a new patch for Ghost of Yōtei with numerous bug and crash fixes, including one that could rarely occur when using ray tracing.
Those who purchased the Digital Deluxe Edition but didn’t receive the Black Ghost Mask…
Scientists at The University of Western Australia’s node of the International Centre for Radio Astronomy Research (ICRAR) have made a remarkable discovery: a massive structure stretching about 185,000 light-years between two galaxies, NGC 4532…
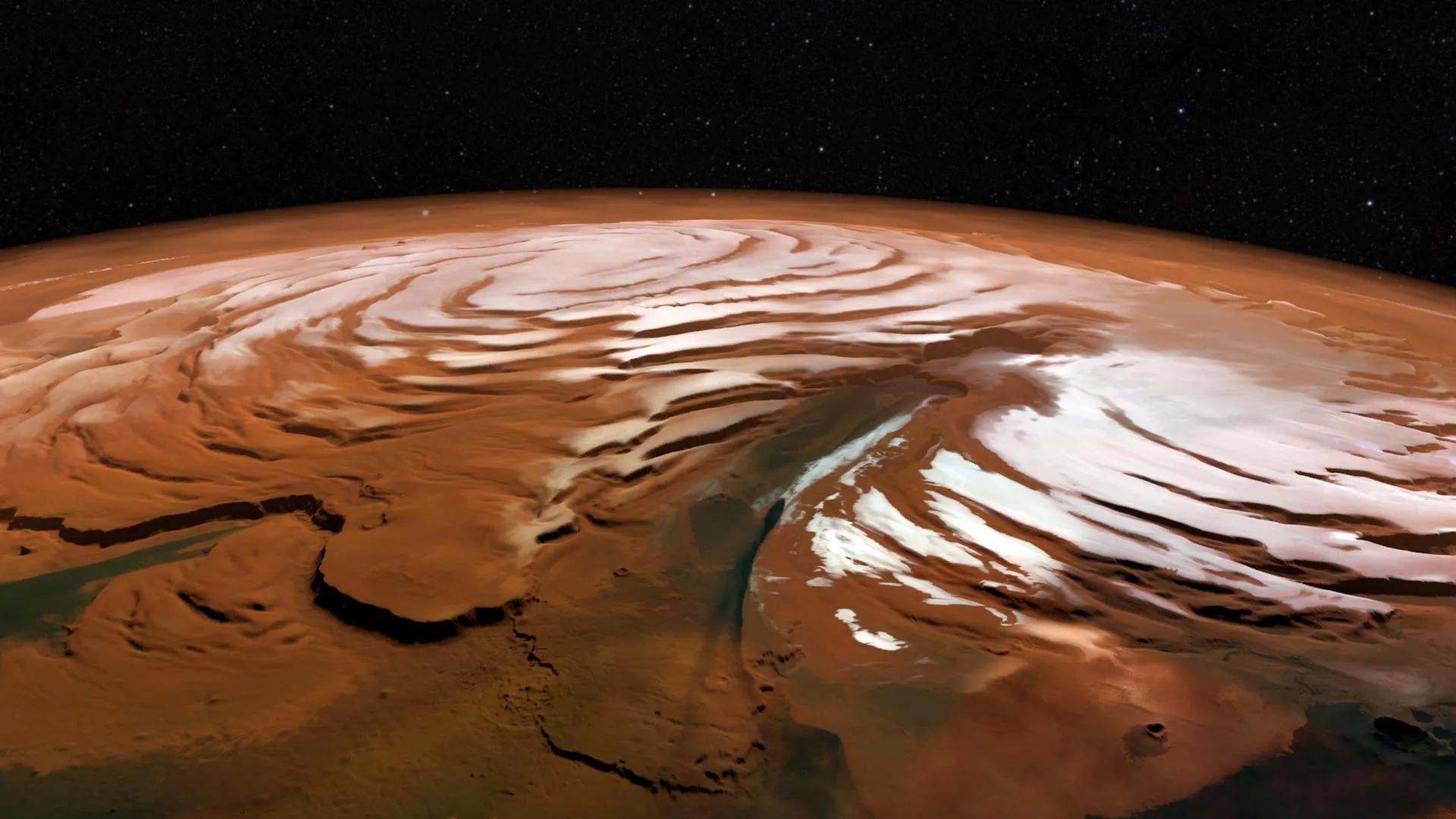
Scientists have recently captured a rare look at the harsh winter conditions swirling above Mars’ north pole. Inside the planet’s polar vortex, temperatures drop dramatically — much colder than the air outside — and the continuous darkness of…
If you wish you could live in the world of Fallout: New Vegas, then you may need Doc Mitchell to take a look at your brain.
However, if the allure of life on the irradiated New Vegas Strip appeals to you that much, you can get a little taste (this…

Relacorilant plus nab-paclitaxel (Abraxane) produced a progression-free survival (PFS) benefit vs nab-paclitaxel alone in a subgroup of patients with platinum-resistant ovarian cancer (PROC) who had received prior PARP inhibitor treatment, including those who had progressed during PARP inhibitor treatment, according to findings from a pre-planned subgroup analysis of the phase 3 ROSELLA trial (NCT05257408), which were presented at the
In the subgroup of patients who had prior exposure to a PARP inhibitor, relacorilant plus nab-paclitaxel (n = 114) elicited a median blinded independent central review (BICR)–assessed PFS of 7.36 months (95% CI, 5.59-8.18) vs 4.63 months (95% CI, 3.55-5.72) with nab-paclitaxel alone (n = 120; HR, 0.60; 95% CI, 0.42-0.85; nominal P = .0035). The investigator-assessed overall response rates (ORRs) in these respective groups were 39.5% and 30.8%.
Furthermore, in the subgroup of patients who had progressed on a prior PARP inhibitor, the BICR-assessed median PFS with relacorilant plus nab-paclitaxel (n = 86) was 7.36 months (95% CI, 5.39-8.44) vs 3.94 months (95% CI, 3.32-5.72) with nab-paclitaxel alone (n = 97; HR, 0.56; 95% CI, 0.37-0.84; nominal P = .0046). The investigator-assessed ORRs in these respective groups were 34.9% and 26.8%.
“Consistent benefit was reported in this subgroup analysis in PARP [inhibitor]–pretreated patients [with] relacorilant plus nab-paclitaxel,” presenting author Domenica Lorusso, MD, PhD, said.
Lorusso is director of the Gynaecological Oncology Unit at Humanitas Hospital San Pio X, as well as a full professor of obstetrics and gynecology at Humanitas University, Rozzano, in Milan, Italy.
Ovarian cancers harbor glucocorticoid receptor expression, which is a marker of poor prognosis. Relacorilant is a novel, selective glucocorticoid receptor antagonist that restores cancer sensitivity to cytotoxic chemotherapy.
ROSELLA enrolled patients with epithelial ovarian, primary peritoneal, or fallopian tube cancer who had an ECOG performance status of 0 or 1, had progressed less than 6 months after their last dose of platinum therapy, and had received 1 to 3 prior lines of therapy, including prior bevacizumab. Patients were randomly assigned 1:1 to receive nab-paclitaxel at 80 mg/m2 on days 1, 8, 15 of each 28-day cycle, in combination with relacorilant at 150 mg on the day before, the day of, and the day after nab-paclitaxel infusion; or nab-paclitaxel monotherapy at 100 mg/m2 on the same nab-paclitaxel dosing schedule.
PFS by BICR and overall survival (OS) served as the dual primary end points. Secondary end points included investigator-assessed PFS, ORR, duration of response, clinical benefit rate, and safety.
Previously, data presented at the
The addition of relacorilant to nab-paclitaxel also showed a trend toward improved OS among patients who had received a prior PARP inhibitor, although these data were only at 50% maturity at the time of this interim analysis.1 The median OS was 15.61 months (95% CI, 12.02-not reached) with relacorilant plus nab-paclitaxel vs 12.58 months (95% CI, 10.09-15.18) with nab-paclitaxel alone (HR, 0.77; 95% CI, 0.53-1.13; nominal P = .1834).
Lorusso noted that relacorilant plus nab-paclitaxel continued to be well tolerated in the prior PARP inhibitor subgroup. Any treatment-emergent adverse effects (TEAEs) were observed in all patients in this subgroup. Among safety-evaluable patients with prior PARP inhibitor exposure who received relacorilant plus nab-paclitaxel, grade 3 or higher TEAEs were seen in 71.1%, and serious AEs were reported in 31.6%. TEAE-related dose reductions of relacorilant (7.0%), dose reductions of nab-paclitaxel (46.5%), treatment interruptions (72.8%), and treatment discontinuations (8.8%) were also observed.
Among safety-evaluable patients with prior PARP inhibitor exposure who received nab-paclitaxel alone (n = 117), grade 3 or higher TEAEs were seen in 64.1%, and serious AEs were reported in 21.4%. TEAE-related dose reductions of nab-paclitaxel (29.1%), treatment interruptions (58.1%), and treatment discontinuations (6.8%) were also observed.
“The safety profile in the trial subgroup was very similar to that [seen in] the overall population,” Lorusso concluded.
Disclosures: Lorusso reported receiving grants from or having contracts with AstraZeneca, Clovis, Genmab, GSK, Immunogen, Incyte, MSD, Novartis, PharmaMar, Seagen, and Roche; receiving consulting fees from AstraZeneca, Clovis Oncology, Genmab, GSK, Immunogen, MSD, PharmaMar, Seagen, and Novartis; receiving payment or honoraria from AstraZeneca, Clovis, Corcept, Genmab, GSK, Immunogen, MSD, Oncoinvest, PharmaMar, Seagen, and Sutro; receiving support for attending meetings and/or travel from GSK, AstraZeneca, Clovis, and MSD; and participating on Data Safety Monitoring or Advisory Boards for AstraZeneca, Clovis, Corcept, Genmab, GSK, Immunogen, MSD, Oncoinvest, PharmaMar, Seagen, and Sutro.
First Fergana Peace Forum was organized from 15 to 16 October 2025 at Fergana university. More than 300 participants from Central Asia, the CIS, Europe, Asia and the America gathered to discuss under the title “Uniting efforts for peace…